If your fracture has been immobilized by a cast, then treatment with a physiotherapist at One Wellness can begin once the cast is removed. While you are in the cast simple finger movements as well as exercises to maintain your shoulder range of motion, such as lifting your arm overhead, will be your only exercises.
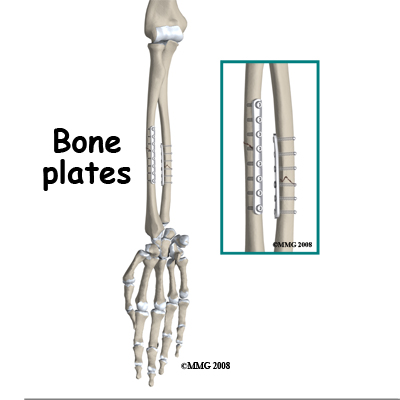
If you have had surgery to fixate your forearm fracture, then rehabilitation at One Wellness will begin as soon as your surgeon recommends it. Each surgeon will set his or her own specific restrictions based on the type of fracture, surgical procedure used, personal experience, and whether the fracture is healing as expected. Generally, however, early non-weight bearing hand, wrist, and elbow movements will be allowed. Your physiotherapist at One Wellness will prescribe these exercises for you and liaise with your surgeon regarding the optimal time to begin more advanced exercises such as putting weight through the healed forearm bone via the hand.
Even if extensive physiotherapy for your forearm is not yet appropriate, at One Wellness we highly recommend maintaining the rest of your body’s fitness with regular exercise. Maintaining general cardiovascular fitness is easy with lower extremity fitness activities such as walking or using a stationary bike or stepper machine. Avid runners may even be able to continue running with clearance from the surgeon. Weights or weight machines for your lower extremity and opposite arm are also acceptable to use as long as the restrictions regarding your healing forearm are strictly abided by. Generally, lifting any weight with your injured limb will not be allowed or will be difficult as your forearm heals so you may require a friend to assist you with your workout setup if you are keen to continue while your bone heals. Your physiotherapist can discuss the most appropriate way for you to maintain your fitness while abiding by your surgeon’s restrictions and can provide a general fitness program specific to your needs.
When the initial cast is removed or immediately after surgery, you may experience some pain when you start to move your wrist, elbow and forearm. If you were immobilized this pain is from not using the joints regularly. If you have had surgery, the pain is likely from the surgical process itself. Your pain may also be from concurrent soft tissue injury that occurred when you fractured your forearm. Your physiotherapist will focus initially on relieving your pain. We may use modalities such as heat, ice, ultrasound, or electrical current to assist with decreasing any pain or swelling you have around the fracture site or anywhere along the arm or into the hand. In addition, we may massage the forearm, wrist, or elbow to improve circulation and assist with the pain.
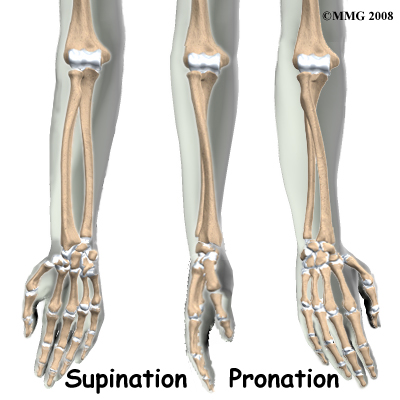
The next part of your treatment will focus on regaining the range of motion, strength, and dexterity in your wrist, hand, elbow, and shoulder. If you have been immobilized, your arm will look and feel quite weak and atrophied after the period of immobilization. Your physiotherapist will prescribe a series of stretching and strengthening exercises that you will practice in the clinic and also learn to do as part of your home exercise program. These exercises may include the use of rehabilitation equipment such as pliable balls or Theraband that provide added resistance for your hand and wrist. We may even give you exercises for your shoulder. The shoulder is the forearm’s link to the rest of the body so it needs to be strong and well controlled for the rest of the upper limb, including the hand, to work well. If necessary, your physiotherapist will mobilize your joints. This hands-on technique encourages the stiff joints of your wrist and elbow to move gradually into their normal range of motion. Fortunately, gaining range of motion and strength after a forearm fracture occurs quickly. You will notice improvements in the functioning of your limb even after just a few treatments with your physiotherapist. As your range of motion and strength improve, we will advance your exercises to ensure your rehabilitation is progressing as quickly as your body allows.
As a result of any injury, the receptors in your joints and ligaments that assist with proprioception (the ability to know where your body is without looking at it) decline in function. A period of immobility will add to this decline. Although your forearm and hand are not traditionally thought of as weight-bearing joints, even an activity such assisting yourself with your arms to get out of a chair or pulling a glass from a cupboard requires weight to be put through or lifted by your forearm and for your body to be proprioceptively aware of your limb. If you are an athlete, then proprioception of your upper extremity is paramount in returning you to sport after a forearm fracture. Your physiotherapist will prescribe exercises for you to regain this proprioception. These might include exercises such rolling a ball on a surface with your hand, holding a weight up overhead while moving your shoulder, or pushups on an unstable surface. Advanced exercises will include exercises such ball throwing or catching. For athletes we will encourage exercises that mimic the quick motions of the sports or activities that you enjoy participating in.
Generally, the strength and stiffness one experiences after a forearm fracture responds very well to the physiotherapy we provide at One Wellness. With our initial one-on-one physiotherapy treatment along with the exercises of your home program, the strength, range of motion, and proprioception gradually improve towards near full recovery/function over a period of 3-6 months even though the actual final stages of bone healing won’t occur for another 6-12 months after that. If your pain continues longer than it should or therapy is not progressing as your physiotherapist would expect, we will ask you to follow-up with your surgeon to confirm that the fracture site is tolerating the rehabilitation well and ensure that there are no hardware issues that may be impeding your recovery.
One Wellness provides services for physiotherapy in Canmore.


 (403) 679-7179
(403) 679-7179  concierge@one-wellness.ca
concierge@one-wellness.ca 

