What treatment options are available?
Nonsurgical Rehabilitation and Treatment
In the case of Sinding-Larsen-Johansson disorder, the disease is often self-limiting, which means that with a certain passing of time, the pain will entirely go away. This time frame coincides with the bone growth plates that form the inferior pole of the patella growing together to form one solid bone. This generally takes one to two years. Once the bones have grown together, the pain and symptoms usually go away completely. Physiotherapy treatment at One Wellness during this time, while the bones are still growing together, can be very useful to manage the injury by decreasing pain and inflammation, as well as to monitor the appropriate level of physical activity that your child partakes in. For true jumper’s knee, where the patellar tendon itself if affected and not the growth plate, physiotherapy is also very useful for the same reasons.
In some cases of jumper's knee, your child may need to stop sports activities for a short period. This allows the pain and inflammation to settle. Usually patients don't need to avoid sports for a long time. ‘Relative rest’ may be suggested rather than a complete cessation of physical activity. ‘Relative rest’ is a term used to describe a process of rest-to-recovery based on the severity of symptoms. If your child is experiencing pain while doing nothing (resting) it means the injury is more severe and your physiotherapist will advise a period of strict cessation of activity. If, however, your child’s pain is not severe and only occurs intermittently with certain activities or after activity, then your child may be able to continue to partake in a moderate amount of activity (relative rest) while being treated for jumper’s knee. Your physiotherapist will provide advice on the appropriate activity level that your child can safely partake in while dealing with their jumper’s knee.
The initial treatment for jumper’s knee at One Wellness will aim to decrease the inflammation and pain in the knee. Simply icing the knee can often assist with the inflammation and relieve a great deal of the pain. In cases of chronic pain (lasting longer than 3 months), heat may be more useful in decreasing pain. Your physiotherapist may also use electrical modalities such as ultrasound or interferential current to decrease the pain and inflammation. Massage, particularly for the quadriceps muscle, may also be helpful.
Medication to ease the pain or inflammation can often be very beneficial in the overall treatment of jumper’s knee. Your physiotherapist may suggest you see your doctor to discuss the use of anti-inflammatories or pain-relieving medications in conjunction with your physiotherapy treatment. Your physiotherapist may even liaise directly with your doctor to obtain their advice on the use of medication in your individual case, and suggest you see them if they feel it would be beneficial.
Cortisone injections performed by a doctor are commonly used to control pain and inflammation in other types of injuries involving the patellar tendon, however, a cortisone injection is usually not appropriate for this condition. Cortisone injections haven't shown consistently good results for jumper's knee and there is also a high risk that the cortisone will cause the patellar tendon to rupture.
Once the initial pain and inflammation has calmed down, your physiotherapist will focus on improving the flexibility, strength, and alignment around the knee joint and entire lower extremity. Static stretches for the muscles and tissues around the knee (particularly the quadriceps and iliotibial band on the outside of the knee) will be prescribed by your physiotherapist early on in your treatment to improve flexibility.
Again, any tightness in the muscles or tissues around the knee can increase the pull on the patellar tendon or affect alignment during walking, running or jumping so it is important to address this immediately. Dynamic stretching (rapid motions that stretch the tissues quickly, similar to that of an eccentric contraction,) will also be taught and will be incorporated into your child’s rehabilitation exercise routine as part of their warm-up when doing more physical activity. Dynamic stretches more effectively prepare the tissues for rapid and repetitive activity than static stretches, which focus more on gaining overall flexibility.
Strength imbalances will also affect the alignment of the knee and can cause muscles to tighten which puts more pressure on the knee and can contribute to the cause of jumper’s knee. Your physiotherapist will determine which muscles in your child’s individual case require the most strengthening. Strength in both the knee and the hip (which controls the knee position) are very important. When bending the knee, as stated above, the patellar tendon is placed under load while it is stretching (eccentric load.) This load can be tremendous especially when jumping and landing. In order to prepare the healing tendon to take this load once your child returns to activity your physiotherapist will prescribe ‘eccentric’ muscle strengthening. Bending the knee quickly into a squatting position and then stopping rapidly (drop squats) encourages the patellar tendon (and entire knee joint) to adapt to the force that will eventually be needed to return to physical activity. When appropriate, weights can be added to simulate the increased body weight that the knee endures during running and jumping.
Your physiotherapist may ask your child to do this exercise on a board slanting downwards (approximately 25 degrees) which has been shown to also increase the force through the tendon. In addition, an electrical muscle stimulator may be used on the quadriceps muscle during the activity which encourages improved recruitment of the muscle, particularly the medial quadriceps portion which has a considerable effect on the position of the patella and pull on the patellar tendon. All exercises should be completed with minimal or no pain and advancing the exercises should be done at the discretion of your physiotherapist as not to flare up the healing tendon. Once these exercise are mastered, your physiotherapist may add even more advanced exercises such as jumping and landing from a height or on different surfaces.
As part of your treatment your physiotherapist may choose to use a hands-on technique to mobilize your kneecap and improve its flexibility. In cases where the patella does not move well, improved movement can change the overall pull on the patellar tendon and therefore assist in decreasing overall pain.
Bracing or taping the knee or kneecap may also help your child do exercises and activities with less pain. Your physiotherapist can educate you on which brace would be most appropriate for your child but an initial trial of taping is an easy and cost-effective way to determine if a brace will in fact decrease your child’s pain before actually investing in one. Your physiotherapist may even teach your child how to tape their own knee or show you how to do it for them. Taping over a longer time frame will cause irritation to the skin and can be cumbersome, therefore if the taping helps, a brace, which performs a similar function, may be suggested. Braces used for jumper’s knee are made of soft fabric, such as cloth or neoprene. There are different types of braces that may help. The braces work by one of two mechanisms. They either work to encourage proper alignment of the patella as it glides down the knee, and therefore decreases the abnormal pull on the patellar tendon, or the brace presses into the patellar tendon itself and distributes the force of the load through a greater region of the patellar tendon. Patients commonly report less pain and improved function with both taping and bracing.
As mentioned above, proper alignment of your child’s entire lower extremity is paramount to decreasing the overall stress that is placed on the patellar tendon. In addition to strengthening, stretching, hands-on treatment, and taping, foot orthotics may be useful to assist with alignment. Foot orthotics can correct a flat foot position, which in turn then encourages proper alignment up the lower extremity chain. Your physiotherapist can advise you on whether orthotics would be useful for your child, and also on where to purchase them.
A critical part of our treatment for jumpers knee at One Wellness includes specific education on returning to full physical activity. Bending and straightening the knee occurs often in everyday activities such as walking or stair climbing so a patellar tendon that is recovering from injury can easily be aggravated. Returning your child back to normal physical activity at a graduated pace is crucial to avoid repetitive pain or a chronic injury. Your physiotherapist will advise you on the acceptable level of activity at each stage of your child’s rehabilitation process and assist your child in returning to his or her activities as quickly and as safely as possible.
With a well-planned rehabilitation program and adherence to suggested levels of rest and activity modification, most children and adolescents dealing with jumper’s knee or Sinding-Larsen-Johansson disorder eventually recover fully without recurring symptoms. By following the rehabilitation plan, most children are also able to partake in a level of activity that suits them while recovering.
One Wellness provides services for physiotherapy in Canmore.
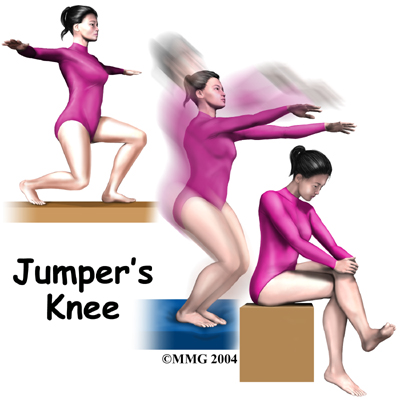 When a child or adolescent complains of pain and tenderness near the bottom of the kneecap, the problem might be from jumper's knee. Kids in sports that require a lot of kicking, jumping, or running are affected most. Repeating these actions over and over can lead to pain in the tendon that stretches over the front of the kneecap (the patellar tendon.)
When a child or adolescent complains of pain and tenderness near the bottom of the kneecap, the problem might be from jumper's knee. Kids in sports that require a lot of kicking, jumping, or running are affected most. Repeating these actions over and over can lead to pain in the tendon that stretches over the front of the kneecap (the patellar tendon.)
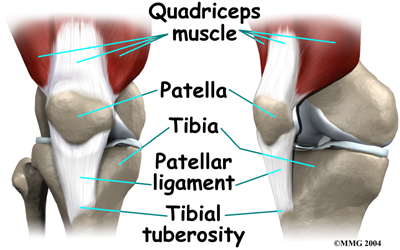 Jumper's knee affects the patellar tendon. The patellar tendon connects the large and powerful quadriceps muscle in the front of the thigh to the tibia (shinbone). The patellar tendon wraps over the front of the patella (kneecap). The upper end of the patellar tendon connects to the bottom tip of the patella. This area is called the inferior pole of the patella. The lower end of the patellar tendon connects to a small bump of bone on the front surface of the tibia. This bump is called the tibial tuberosity.
Jumper's knee affects the patellar tendon. The patellar tendon connects the large and powerful quadriceps muscle in the front of the thigh to the tibia (shinbone). The patellar tendon wraps over the front of the patella (kneecap). The upper end of the patellar tendon connects to the bottom tip of the patella. This area is called the inferior pole of the patella. The lower end of the patellar tendon connects to a small bump of bone on the front surface of the tibia. This bump is called the tibial tuberosity. In addition to overuse of the tendon causing the patellar tendon pain, abnormal alignment of the lower limbs can play a major part in the development of jumper’s knee. Kids who are knock-kneed or flat-footed seem to be more prone to the condition. These altered postures cause a sharper angle between the quadriceps muscle and the patellar tendon. This angle is called the Q-angle. Having a large Q-angle puts more tension on the patellar tendon and the risk of developing jumper's knee is thus higher.
In addition to overuse of the tendon causing the patellar tendon pain, abnormal alignment of the lower limbs can play a major part in the development of jumper’s knee. Kids who are knock-kneed or flat-footed seem to be more prone to the condition. These altered postures cause a sharper angle between the quadriceps muscle and the patellar tendon. This angle is called the Q-angle. Having a large Q-angle puts more tension on the patellar tendon and the risk of developing jumper's knee is thus higher.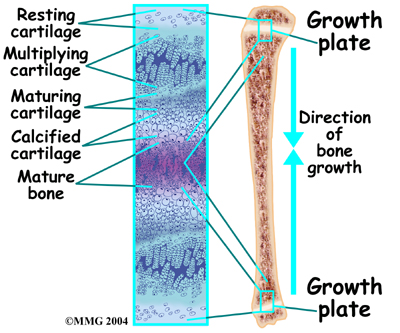 Sinding-Larsen-Johansson disorder is part of a category of bone development disorders known as the osteochondroses. (Osteo means bone, and chondro means cartilage.) In normal development, specialized areas called growth plates change over time from cartilage to bone. The growth plates expand and unite. This is how bones grow in length and width. Bone growth centers are located throughout the body.
Sinding-Larsen-Johansson disorder is part of a category of bone development disorders known as the osteochondroses. (Osteo means bone, and chondro means cartilage.) In normal development, specialized areas called growth plates change over time from cartilage to bone. The growth plates expand and unite. This is how bones grow in length and width. Bone growth centers are located throughout the body.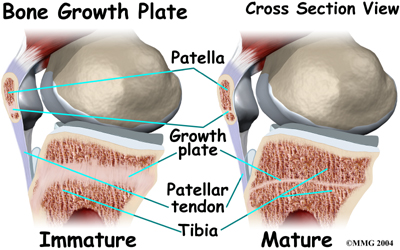
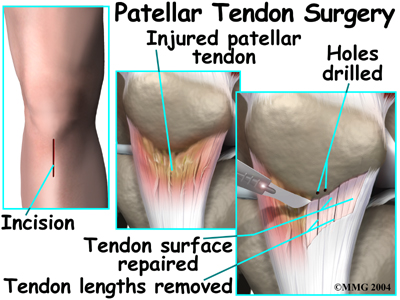 The skin is opened to expose the patellar tendon. Next, the surgeon carefully peels damaged tissue off the surface of the tendon. Three to five thin lengths of the tendon are removed. In some cases, small drill holes are made in the bottom tip of the patella. This drilling causes a small amount of bleeding, which signals the body to begin to heal the area. The surgeon also removes any damaged tissue nearby the area before completing the operation by stitching up the skin and wrapping the area with a bandage.
The skin is opened to expose the patellar tendon. Next, the surgeon carefully peels damaged tissue off the surface of the tendon. Three to five thin lengths of the tendon are removed. In some cases, small drill holes are made in the bottom tip of the patella. This drilling causes a small amount of bleeding, which signals the body to begin to heal the area. The surgeon also removes any damaged tissue nearby the area before completing the operation by stitching up the skin and wrapping the area with a bandage.
 (403) 679-7179
(403) 679-7179  concierge@one-wellness.ca
concierge@one-wellness.ca 

