Physiotherapy treatments at One Wellness are a critical part of recovery and rehab from this injury. The first goal is to reduce pain and interrupt the inflammatory cycle. Next our treatments are directed at getting the muscles to relax in order to help you regain the motion and function of your shoulder. The overall goal of physiotherapy is to help you regain full range of motion in the shoulder.
If your pain is too strong at first to begin working on shoulder movement, your physiotherapist may need to start with treatments that focus on pain control. The use of ice, heat, ultrasound, and other electrical modalities may be useful at this stage. Your therapist may also use massage and gentle mobilizations to ease muscle spasm and pain. If your doctor has prescribed it, iontophoresis may also be used. Iontophoresis is a way to push medications through the skin directly into the inflamed tissue by using an electrical modality to apply the medication.
As soon as possible your therapist will begin to work on regaining your shoulder’s movement, even if that range of movement is only small at first. Your sessions may begin with treatments such as moist hot packs, ultrasound or massage, which help to relax the muscles and get the shoulder tissues ready to be stretched. Your physiotherapist will assist you in stretching your shoulder through the available ranges of motion, but they will also show you stretches that you can do on your own as part of a home program. Using an overhead shoulder pulley in the clinic and as part of a home program is extremely useful in gaining shoulder range of motion. Doing pendular exercises can also assist with pain at this stage, and help to maintain some shoulder range of motion. Pendular exercises are performed by leaning forward or to the side, letting the arm hang clear of the chest, and then initiating movement with your trunk so that the dangling limb passively and gently moves. This action provides some traction to the glenohumeral joint (shoulder joint), which aids in pain relief, and also assists the shoulder into a relative elevated motion (in relation to the trunk.) It is important that the pendular activity is done as passively as possible without initiating motion from the shoulder muscles. The exercise should look similar to a weighted pendulum that randomly swings on the end of a piece of string.
If your doctor recommends an injection of a long-acting anesthetic with cortisone for your shoulder, you should plan on seeing your physiotherapist at One Wellness right after the injection. The extra fluid from the injection stretches out the tissues of the joint capsule so an aggressive session of stretching right after an injection can help maximize the stretch to the joint capsule. Your physiotherapist can liaise with your doctor regarding a planned injection in conjunction with a stretching session.
Maintaining your neck range of motion is also very important when your shoulder is not moving well, so your therapist will also prescribe exercises to ensure you can move your neck well for all your daily activities, and that you don’t end up with a stiff neck along with your stiff shoulder.
The next part of your treatment at One Wellness will involve mobilizing the joints of your shoulder, including your glenohumeral joint, the joint of the shoulder blade and the thorax (scapulothoracic joint), and even the joints where your collarbone joins the trunk and the shoulder (sternoclavicular and acromioclavicular joints.) Your physiotherapist will passively move these joints into their available ranges of motion while you relax the muscles of your shoulder completely.
Interestingly, the strength of your shoulder is often maintained in primary adhesive capsulitis, especially once you pass the stage of having pain and are simply restricted because of the range of motion. As you gain more range of motion, however, you will notice weakness in the shoulder in these ranges of movement simply because you have not used the shoulder in these ranges for an extended period of time. For this reason, your therapist will focus more on strengthening exercises in the later stages of your rehabilitation, once your pain is under control and your shoulder range of movement is improving.
With secondary adhesive capsulitis there may be significant weakness in the shoulder due to the original injury that started the process in the first place (ie. shoulder impingement or rotator cuff tear.) In these cases, your therapist will start by prescribing simple strengthening exercises. Initially this will only involve isometric strengthening. Isometric strengthening exercises are done by tightening your muscles without actually moving the associated joint. Isometric exercises work the muscles without straining the injured or painful tissues. Your physiotherapist will teach you how to use your other hand or a wall for resistance while you flex and tighten your muscles, creating an isometric contraction of the shoulder muscles. Your therapist will then progress your exercises so that you are strengthening the muscles through their available ranges of motion as you regain these motions. This may involve using light-weights or Theraband to add resistance for your upper limb. Adequate strength and endurance in the rotator cuff muscles throughout a variety of ranges of motion, including over shoulder height, is needed to ensure full functioning of the shoulder.
As a result of any injury, the receptors in your joints and ligaments that assist with proprioception (joint sense of position) decline in function. A period of immobility will add to this decline. Although your arm and shoulder girdle are not traditionally thought of as weight-bearing parts of the body, even an activity such as assisting yourself with your arms to get out of a chair or pulling a glass from a cupboard requires weight to be put through or lifted by your shoulder girdle and for your body to be proprioceptively aware of your limb.
The proprioceptive control of the scapula on the rib cage (scapulothoracic motion) is especially important in being able to use your shoulder girdle and upper limb effectively without causing further injury. Normal scapulothoracic motion is particularly essential once you are able to use your limb near or above shoulder height. For this reason, your physiotherapist will teach you how to properly control your scapula during everyday activities as well as during your rehabilitation exercises. Your physiotherapist will also remind you about maintaining good shoulder posture even when sitting or using your upper limb in activities below shoulder height, such as working on the computer.
Rounded shoulders in this position crowds the shoulder joint and can lead to or prolong shoulder impingement and pain. Regaining proprioception of the shoulder girdle and upper limb requires concentrated work, as most people have not previously needed to focus so intently on such controlled motions. The concentrated effort, however, has a substantial reward, as good scapulothoracic control is the key to avoiding further shoulder problems once your adhesive capsulitis has been rehabilitated.
Proprioceptive exercises might include activities such as rolling a ball on a surface with your hand, holding a weight up overhead in lying while you move your shoulder, or pushups on an unstable surface. Advanced exercises may include activities such as ball throwing or catching overhead once you gain that range of motion.
As mentioned above, adhesive capsulitis can unfortunately be a slow problem to resolve. You may need therapy treatments for three to four months or longer before you get full shoulder motion and function back, and you will need to also continue your home exercise program for at least as long.
If conservative treatment at One Wellness is not progressing as quickly as your physiotherapist would expect, then more aggressive intervention may be required.
One Wellness provides services for physiotherapy in Canmore.

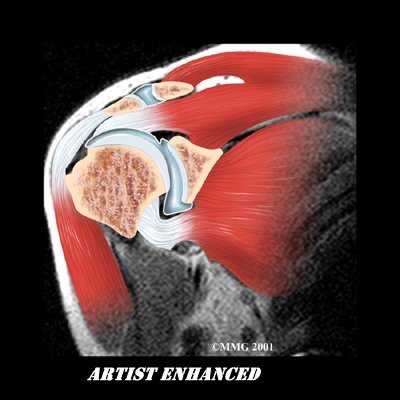
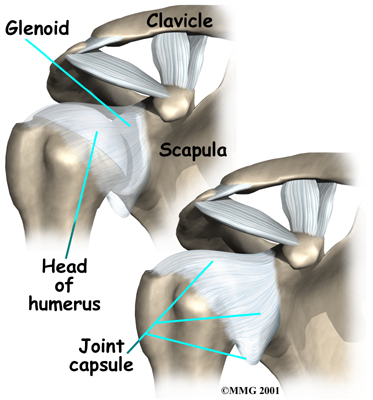 The shoulder is made up of three bones: the scapula (shoulder blade), the humerus (upper arm bone), and the clavicle (collarbone). The joint capsule is a watertight sac that encloses the joint and the fluids that bathe and lubricate it. The walls of the joint capsule are made up of ligaments. Ligaments are soft connective tissues that attach bones to bones. The joint capsule has a considerable amount of slack (loose tissue), so the shoulder is unrestricted as it moves through its large range of motion.
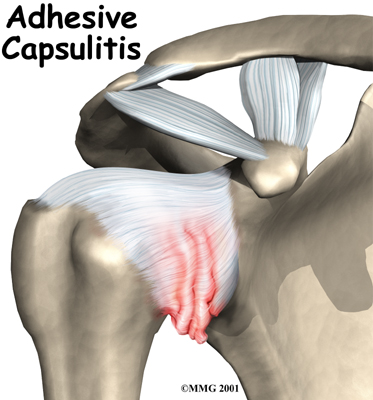
The shoulder is made up of three bones: the scapula (shoulder blade), the humerus (upper arm bone), and the clavicle (collarbone). The joint capsule is a watertight sac that encloses the joint and the fluids that bathe and lubricate it. The walls of the joint capsule are made up of ligaments. Ligaments are soft connective tissues that attach bones to bones. The joint capsule has a considerable amount of slack (loose tissue), so the shoulder is unrestricted as it moves through its large range of motion.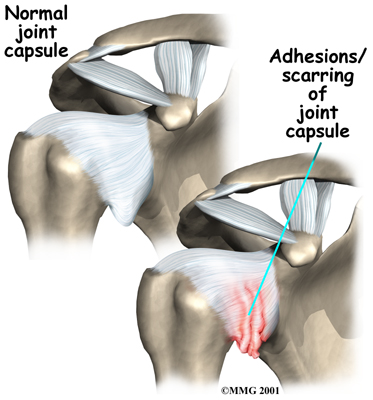 As the name suggests, adhesive capsulitis affects the fibrous ligaments that surround the shoulder forming the capsule. The condition referred to as a frozen shoulder usually doesn't involve the capsule. Secondary adhesive capsulitis (or true frozen shoulder) might have some joint capsule changes but the shoulder stiffness is really coming from something other than the joint capsule. Some of the conditions associated with secondary adhesive capsulitis include rotator cuff tears, biceps tendinitis, and arthritis. In either condition, the normally loose parts of the joint capsule stick together. This seriously limits the shoulder's ability to move, and causes the shoulder to relatively freeze.
As the name suggests, adhesive capsulitis affects the fibrous ligaments that surround the shoulder forming the capsule. The condition referred to as a frozen shoulder usually doesn't involve the capsule. Secondary adhesive capsulitis (or true frozen shoulder) might have some joint capsule changes but the shoulder stiffness is really coming from something other than the joint capsule. Some of the conditions associated with secondary adhesive capsulitis include rotator cuff tears, biceps tendinitis, and arthritis. In either condition, the normally loose parts of the joint capsule stick together. This seriously limits the shoulder's ability to move, and causes the shoulder to relatively freeze.
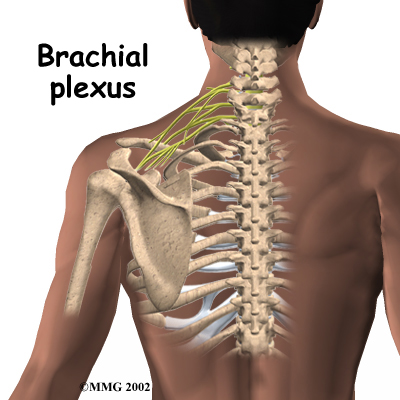 As with any procedure, MUA has risks. There is a very slight chance that the aggressive stretching can injure the nerves of the brachial plexus, which is the network of nerves running to your arm. There is also a risk of fracturing the humerus (the bone of the upper arm), especially in people who have osteopenia or
As with any procedure, MUA has risks. There is a very slight chance that the aggressive stretching can injure the nerves of the brachial plexus, which is the network of nerves running to your arm. There is also a risk of fracturing the humerus (the bone of the upper arm), especially in people who have osteopenia or 
 (403) 679-7179
(403) 679-7179  concierge@one-wellness.ca
concierge@one-wellness.ca 

