Physiotherapy at One Wellness will help immensely with any tendon problem you have, whether acute or chronic. Beginning treatment with us as early as you can once you develop the problem is the best way to guarantee that the problem resolves and that it does not become chronic.
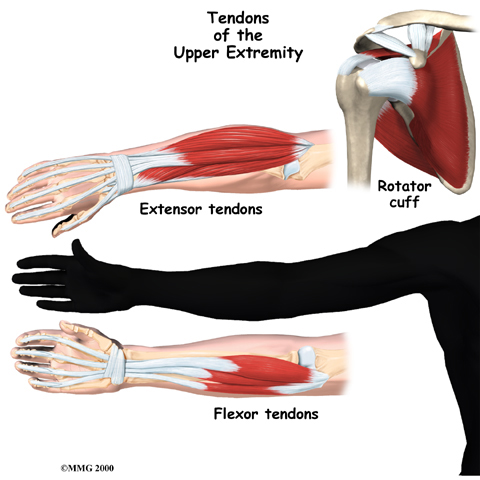
On your first visit to One Wellness your physiotherapist will ask you questions about where precisely the pain is, when the pain began, what you were doing when the pain started, and what movements aggravate or ease the pain. If you are involved in sport, your training history including any increases in frequency or intensity of activity or change in equipment will also be important for us to inquire about. If you have not seen your doctor, and your problem has not been identified, then the history alone will often lead your physiotherapist to your tendon being the source of your pain.
Next your physiotherapist will do a physical examination of the area around the tendon as well as your entire associated limb and other joints near the area. Your physiotherapist will assess your postural alignment, flexibility and joint laxity with regards to the closest joint and may want to look at how you stand or sit. If the tendon is in your lower extremity, they will also observe your foot position and watch you walk, and possibly squat, run, or jump. If you are involved in sport, they may also ask you to bring in some of your equipment to the next appointment, such as your running shoes or tennis racket, so it can be examined for potential faults or factors that may be contributing to the development of your pain.
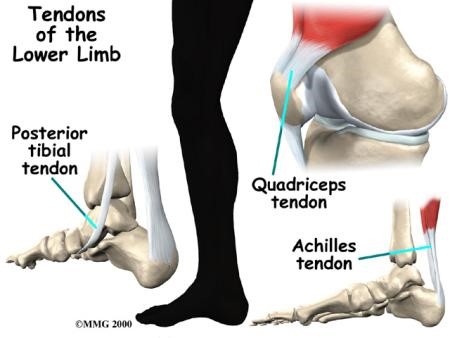
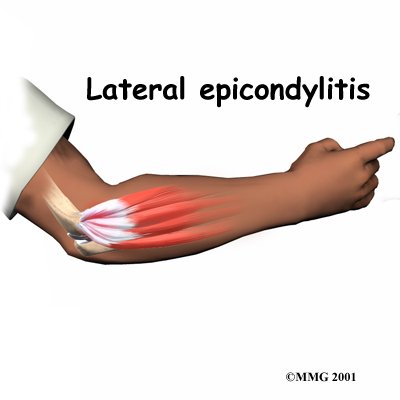
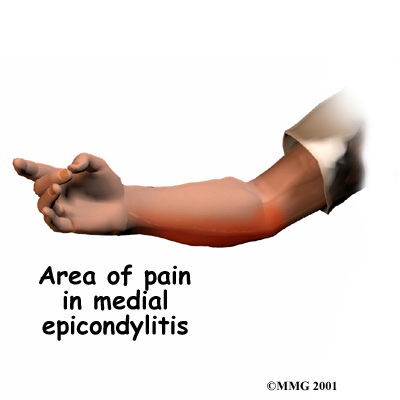
Next your physiotherapist will check the strength and lengths of the muscles directly attaching to your painful tendon as well as any other related muscles. If any muscles are weak or tight, they can contribute to the stress on the related tendon. Often joints that may seem unrelated to the problem to you will need to be assessed by your physiotherapist as weaknesses or imbalances in and around other areas frequently contribute to the pain that arises in a tendon of the associated arm or leg. For instance, the grip strength of your hand may be tested even if it is your elbow that is causing your pain, or the strength around your hip may be assessed if your Achilles tendon is the issue.
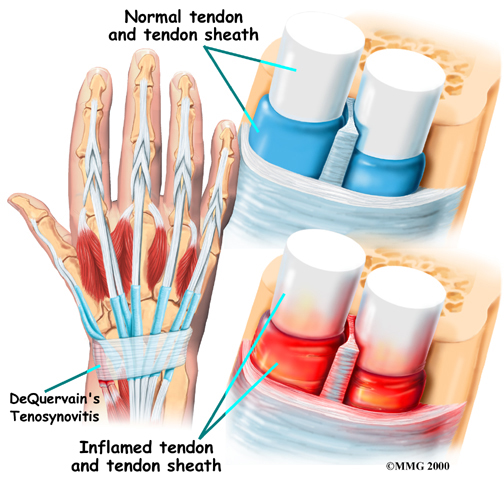
Initially the treatment at One Wellness will focus on decreasing any inflammation and pain around your tendon. Your physiotherapist may use electrical modalities to do this such as ultrasound or interferential current. Heat and/or ice can also be very useful at any stage of tendon healing to decrease pain and also inflammation if there is any. Your physiotherapist can advise you on whether heat or ice or both is the best treatment in your particular case. Your physiotherapist may also use massage for the muscles around the tendon or even directly over the tendon to ease your discomfort and again assist with decreasing any inflammation if it is present.
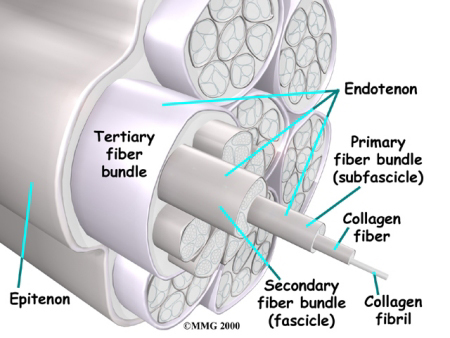
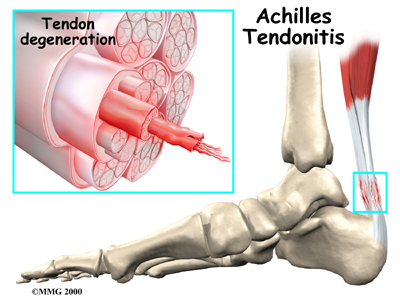
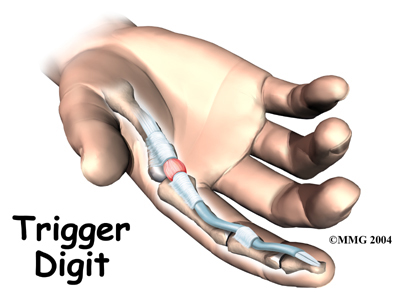
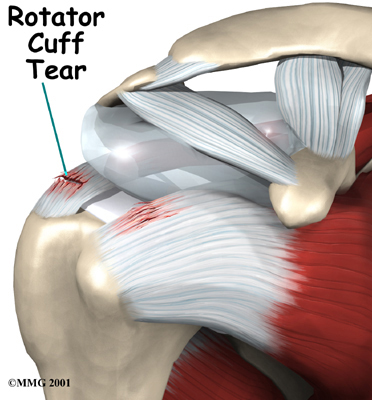
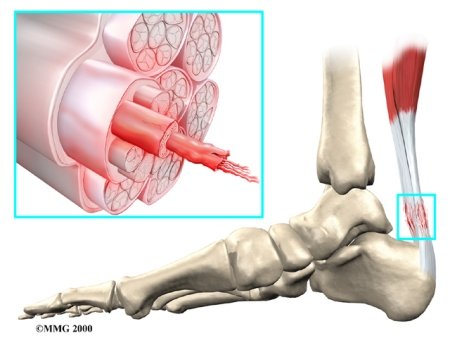
A crucial component to the healing of any tendon injury is relative rest. As most tendon injuries result due to repetitive activities over time that cause too much stress on the tendon and then lead to pain, your physiotherapist will strongly advise you to avoid any activities that cause you discomfort. This may mean, for instance, if it is a tendon in your elbow that is affected, that you have to use your other arm as often as possible to give the painful tendon a period of relative rest. This may also mean resting for a short period from any sport you do, or at least decreasing the amount you play over a period of time. Your physiotherapist will specifically guide you regarding the needed rest for your individual injury. This rest may seem quite difficult to achieve, however it is well known that generally without relative rest for an injured tendon, there is little chance for it to heal and the problem can easily become chronic, or can lead to a more severe injury, such as a tear in the tendon. A period of rest where the tendon is not being aggravated also greatly improves the ability of any medication you may be taking along with the physiotherapy treatment you are receiving to assist the healing of the injury. This rest period allows a short time frame where the tendon is not being aggravated while at the same time, it is also receiving the necessary treatments to expedite healing of the tendon. After your period of rest your physiotherapist will advise you when it is safe to slowly start back at your activity.
There are many braces on the market that are designed to assist with the rehabilitation of tendonitis injuries. There is basically a brace for all potential areas of tendonitis in the body including areas such as the Achilles, elbow and wrist. Your physiotherapist can advise you regarding whether a brace would be useful in your case, and can also advise you on where to purchase them. Quite often your physiotherapist will trial some strapping or taping prior to you investing in a brace for the affected area. Taping the area is obviously cheaper than a brace, and gives you and your physiotherapist a good idea as to whether a brace would help with your pain. Tape, although often helpful, can not often be used for long periods or repetitive treatments because the skin gets irritated, and in addition it may be difficult for you to tape the area independently when you are not at One Wellness. For this reason, a brace is often recommended.
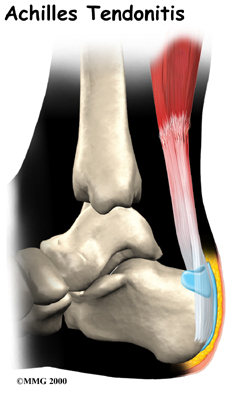
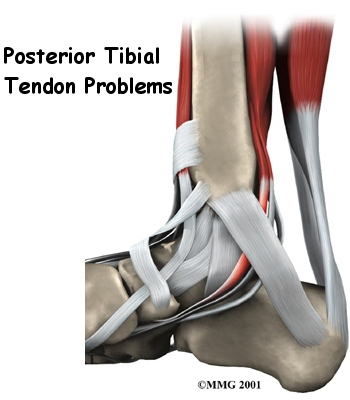
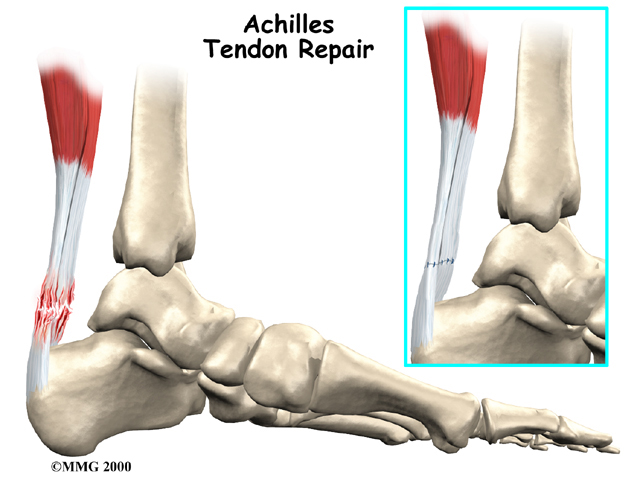
In certain tendon problems, such as Achilles tendonitis, other types of orthotics may be suggested. The pain associated with Achilles tendonitis often responds well to a heel insert that lifts the heel of the affected side, and shortens the relative length of the tendon. This in essence decreases the stretch on the tendon and can often be enough to allow some relative rest for the injured area.
In the case of any lower extremity tendon issue, shoe orthotics may also be suggested by your physiotherapist. Poor alignment of the lower extremity will put undue stress on the tendons of the lower extremity. Correcting the position of your foot, if it is a contributing factor to this misalignment, will decrease this stress and will also assist the healing process of the tendon.
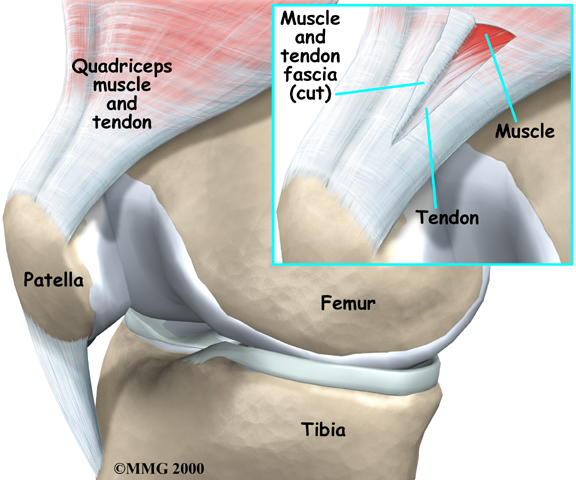
During the next part of treatment your physiotherapist will prescribe stretching and strengthening exercises for your affected area. Your physiotherapist may do some stretching for you in the clinic, but they will also teach you how to stretch the affected area as well as any related muscles as part of your home program. Strengthening the affected tendon and associated muscles will also be a part of your home program. Initially strengthening will be simple exercises and may or may not include using any weights. As soon as appropriate, however, your physiotherapist will prescribe eccentric exercises which are crucial to making a full recovery from a tendon injury.
Eccentric contractions occur as the muscle lengthens and the tendon is put under stretch. Landing from a jump is an example of an eccentric contraction for the knee or Achilles tendon. These types of contractions encourage the tendon to adapt to the more aggressive force that will eventually be needed to return to regular physical activity.
Adding weights to these exercises as well as doing the exercises in a speeded fashion will also encourage the tendon to adapt to the more aggressive forces that it will need to endure repetitive activities of daily living or sporting activities. All exercises should be completed with minimal or no pain and advancing the exercises should be done at the discretion of your physiotherapist as not to flare up the healing tendon.
Maintaining proper posture and alignment of your body during regular everyday activities can also greatly affect how quickly your tendon heals. For upper extremity issues, good sitting posture is vital in order to decrease the stress on the arms, neck and back.
Shoulders should remain upright and out of the slouched position as this puts stress on the neck, upper back, and shoulders, and in turn affects how well you can use your arm. If you are frequently using a computer, the position of your hand on the keyboard or mouse over a prolonged period can also add stress to your tendons and accentuate the problem. Your physiotherapist will advise you regarding your posturing as well as make suggestions for ergonomic tools that may help you decrease the stress on your tissues and encourage more rapid healing. If you are a manual worker the amount of lifting and gripping involved in your day will be assessed. Excessive gripping or lifting especially without having good grip (ie: using too large or poorly gripped gloves) will add to the strain on your injured body part, so changes to these activities in your everyday life will be suggested.
For lower extremity issues, the alignment of your hips over top of your feet can add to or decrease the stress that is put through your injured area. Your physiotherapist will advise you on proper alignment of your hips, knees, ankles and feet, and will encourage you to maintain and use this posture throughout your day even during simple activities such as walking or climbing stairs. These simple changes can make a massive difference to the cumulative stress that is placed on your painful tendon.
As soon as it is appropriate your physiotherapist will integrate you back into the activities that you were having difficulty doing, whether that be typing on the computer, or playing high-level sport. A period of controlled and supervised slow reintegration is crucial to avoid further pain or a flare up of the healing area.
Most people with acute or chronic tendon problems, with the help of physiotherapy at One Wellness, are relieved of their pain and can eventually take part in their normal activities. In a few cases, however, a high level of pain lingers on even after the appropriate rest and a significant amount of therapy. For these patients, a more aggressive form of treatment will need to be considered. In these cases, your physiotherapist will refer you back to your doctor. A relatively new form of treatment may be available to you called platelet rich plasma injections (PRP.) Platelet-rich plasma refers to a sample of serum (blood) plasma that comes from the patient themselves, and is treated to extract as much as four times more than the normal amount of platelets. Platelets are the smallest cells in the blood and are essential for blood clotting and injury healing. This serum is then injected back into the problem area to encourage new tissue healing. PRP treatment enhances the body’s natural ability to heal itself and can shorten recovery time from acute and chronic soft tissue injuries.
If no other conservative treatment is successful, surgery may be necessary to debride the degenerative tendon and encourage new healing. Surgery can be very successful in treating the problem of chronic tendon pain but ongoing rehabilitation after surgery will be necessary to ensure complete success. If surgery is necessary for your tendon problem, your physiotherapist at One Wellness can guide you through the appropriate post surgical rehabilitation necessary that is specific to your injury and your individual requirements in order to return you as quickly as possible back to your everyday and sporting activities.
One Wellness provides services for physiotherapy in Canmore.
Portions of this document copyright MMG, LLC.


 (403) 679-7179
(403) 679-7179  concierge@one-wellness.ca
concierge@one-wellness.ca 

