What are the potential complications of this fracture?
Complications are events or conditions that make the process of recovering from the fracture more complex. Although most complications are rare, much of the management of the injury is directed at avoiding complications, detecting them early and treating them if they occur. Doctors, nurses and physiotherapists will ask patients to move their fingers right after an operation on the wrist as these early movements can help to detect early complications.
Malunion
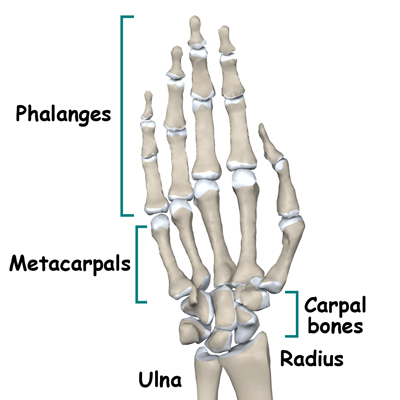
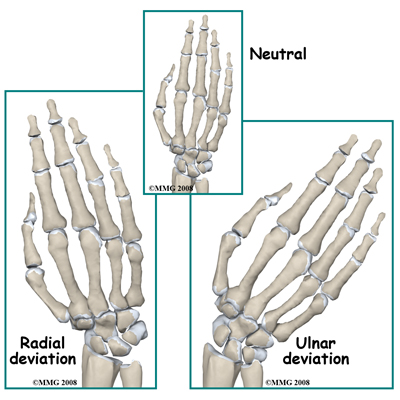
The term malunion implies that the fracture has healed but is not in the correct anatomic position. There are three aspects of malunion of distal radius fractures that give rise to concern 1) irregularity of the distal radius joint surface, 2) tilting of the joint surface, and 3) shortening of the radius. A gap or step in the joint surface greater than 1 mm is a cause for concern as it increases the long-term possibility arthritis of the joint.
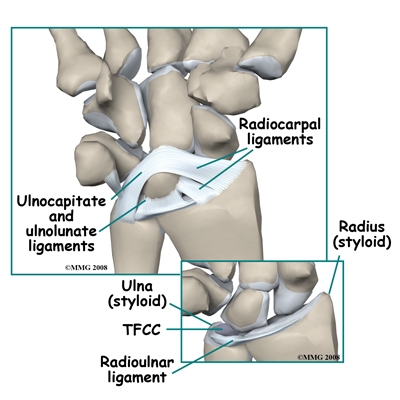
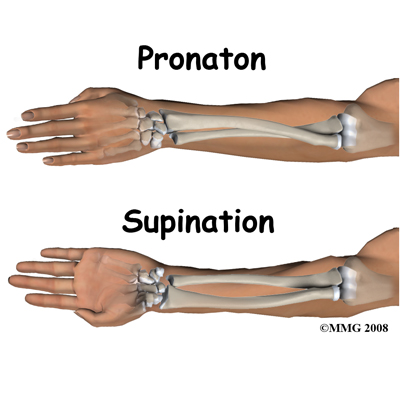
Post-traumatic arthritis of the joint is actually quite rare and there is still no absolute certainty about the amount of irregularity that will cause it. Most doctors agree, however, that an irregular joint surface should be avoided if possible. Tilt of the distal radius is even more difficult to evaluate. A severe degree of tilt affects the distal radioulnar joint and rotation of the forearm. Although, once again, there is no consensus, many doctors prefer to avoid a high angle of tilt and would operate to prevent it.
Shortening of the radius results in impingement between the ulna and the carpal bones, which is often painful.
Preventing malunion is important, as the treatment for it is difficult. Once the bone is healed it is a major undertaking to "take down" the fracture by surgery and fix it into a better position. A "wait and see" approach is often preferred rather than an immediate surgical procedure to fix a malunion. If another surgery is required, there are various operations used for reconstruction of a painful or poorly functioning wrist.
Nerve Injury
The median and ulnar nerves are often compressed by the impact of a fall and may be damaged to the extent that their function is affected. Once this is established it may be necessary to decompress the nerve. Recovery after this surgery is usually complete but delay in treating a nerve injury should be avoided. If you have numbness in your hand after a fracture you must immediately inform your doctor about it.
Another source of nerve injury is from the hardware used to treat the fracture. Pins inserted through the skin may come close to or penetrate into nerves that pass over the fracture. The radial nerve on the thumb side of the wrist is quite vulnerable to this type of injury. It causes pain similar to an electric shock and may also cause numbness, however most often this resolves when the pin is removed. Damage to a nerve may also result in a sensitive, tender scar.
Compartment Syndrome
Fractures of the distal radius cause damage to the muscles of the forearm and involve bleeding into the muscle compartments. Both these processes cause increased pressure in the muscle compartments, which may be further increased by bandages or casts. If the pressure gets too high the blood supply of the muscle tissue is impaired causing further damage and a further increase in intra-compartment pressure.
The hallmark symptom of compartment syndrome is relentlessly increasing pain made worse by active or passive finger movements. For this reason patients are encouraged to move their fingers as soon as possible so any unwarranted pain can be detected. If it is only mildly uncomfortable this is evidence against a compartment syndrome. Once established, compartment syndrome tends to get worse and cause muscle death with long lasting disability. The treatment is to immediately operate to open up the muscle compartments and relieve the pressure (fasciotomy). If this is done before any muscle dies the results are excellent although the scars on the forearm may be dramatic.
Infection
If the skin is wounded either by the accident (causing an open fracture) or by surgery there is a chance that bacteria will infect the wound. Antibiotics are often routinely prescribed to reduce the chance of this happening. The risk of an infection following an operation with modern treatment is less than 2% (one in 50) but this is little consolation to you if you do get an infection.
Signs and symptoms of an infection include increased wound swelling, increased redness, increased tenderness, and the possibility of pus draining from the wound. It is normal to have a slight fever after an operation but with an infection this tends to go up and lasts longer. Cultures taken of the blood or drainage from the wound may reveal the bacteria responsible and assist in treatment.
The mainstay of treatment is the prolonged use of high-dose bacteria-specific antibiotics but further surgery is also very common. With surgery the wound is opened and washed out to reduce the number of bacteria and give the antibiotics a fighting chance. Sometimes the wound may be packed with antibiotic beads to increase the local concentration of the drug. Once the infection is under control the fracture should heal, however it may be necessary to remove all the metal implants as bacteria tend to grow on foreign material.
In the majority of cases the combination of early aggressive antibiotic treatment, wound washout, and removal of the hardware once the fracture is healed is successful in restoring the wrist to normal after an infection.
Complex Regional Pain Syndrome (CRPS)
This troublesome problem results in burning pain, swelling, and stiffness of the hand and wrist even though the fracture has healed. Normally after an injury the blood supply is increased to the injured area as part of the body's marshaling of resources. Generally this increase only lasts a few days post-injury and then the blood supply returns to normal levels. After some wrist fractures, however, this does not happen and the increased blood supply causes prolonged swelling. This in turn makes it difficult to move the hand and wrist. As a result everything stiffens up and attempts to move the wrist are unusually painful.
It is not clear why CRPS occurs although there is a connection between pain and the blood supply reflex. CRPS was previously called Reflex Sympathetic Dystrophy (RSD) so this term may still be used but refers to the same process. The pumping action of the muscles helps to reduce swelling therefore CRPS is less common if you get the fingers, hand and wrist moving early. This is another reason why you are asked by the physiotherapist and other health care professionals to move your fingers right away.
Treatment of established CRPS is different for different individuals but includes exercises prescribed by a physiotherapist, splints to eliminate the stiffness, medication for the pain, and compression gloves to help reduce the swelling. Nerve blocks may be helpful both for diagnosis and treatment. The prognosis of CRPS is good with most people recovering, however it may take a long time for complete recovery to occur.
Hardware Failure
Most implants that are used to stabilize fractures are made of metal and therefore subject to metal fatigue. Metal fatigue is a similar process as to when you want to shorten a piece of wire and so to do this you repeatedly bend it back and forth until it breaks. A metal implant, such as a wire or a plate that crosses over an unhealed fracture, also bends. This movement is very small but "micromovement" does occur at fractures and the stress is transmitted to the implant. Once the fracture is healed this micromovement stops and there is almost no load on the hardware. It is a race between the bone healing and the implant breaking, which, in most cases, is won handily by the healing process.
Unfortunately, under some circumstances the hardware does fatigue and fail. If you carry loads or use vibrating machinery before the fracture is healed, this greatly increases the tendency of fatigue failure. The restrictions on activities such as lifting weights or riding a motorcycle too early may seem unnecessary or overcautious when your wrist is feeling strong and comfortable and when these activities do not hurt, however, the restrictions are based on the length of time it takes the bone to heal.
Until the bone is healed loading the hardware may have unexpectedly serious results. The risk of fatigue failure is also increased by smaller implants, with delay in healing, and with infection. Gaps between the bone fragments may also increase the tendency of the metal to fatigue.
If the implant does break the bone may still heal in the current position if protected by a cast (and if you stop the activities that loaded it). Alternatively, surgery may be repeated using a bone graft, which promotes healing and stabilizes the fracture. Luckily, in the long term this complication is often seen as a "bump in the road" as the measures to heal the fracture usually succeed in the end.
Other Hardware Problems
Pins, plates and screws are often used in the surgical treatment of distal radius fractures. The location of these items of hardware often means that the tendons that pass to the hand need to glide over the plate or the protruding ends of the pins and screws. In a small percentage of cases the tendons are irritated and may even rupture. This is a relatively common complication of plates on the back of the wrist where there isn't much room for the tendons. The main symptoms are pain in the wrist region when moving the fingers or thumb, and tenderness to the touch. If the tendon does rupture this will generally affect one specific movement such as straightening the thumb or index finger. The treatment for this complication is to remove the hardware that is causing the trouble. If the fracture is not healed, however, some other method of treatment may be necessary such as moving the plate to a different surface or into a different position.
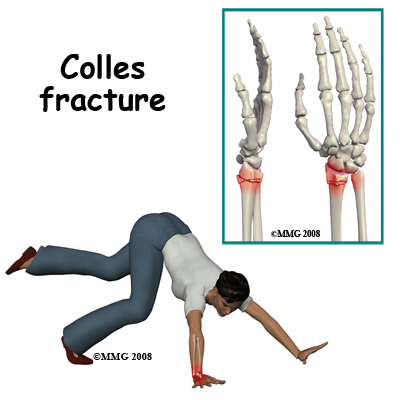
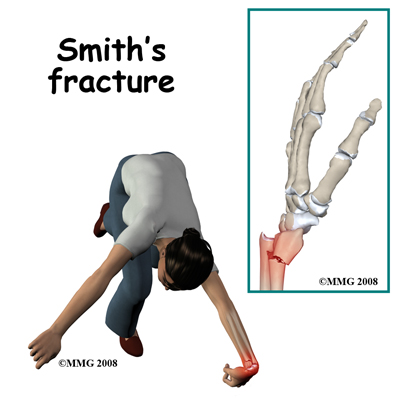
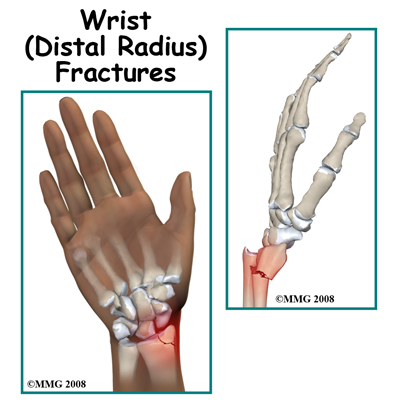 Fractures of the wrist are common injuries. When you fall, it is only natural to put your hand out to break the fall and prevent more serious injuries to your face and body. The forces that go through your wrist when you fall on your outstretched hand are many times the weight of the body. Conditions that make a fall more likely, such as icy, wet, or uneven surfaces can increase the risk of a wrist fracture.
Fractures of the wrist are common injuries. When you fall, it is only natural to put your hand out to break the fall and prevent more serious injuries to your face and body. The forces that go through your wrist when you fall on your outstretched hand are many times the weight of the body. Conditions that make a fall more likely, such as icy, wet, or uneven surfaces can increase the risk of a wrist fracture.

 (403) 679-7179
(403) 679-7179  concierge@one-wellness.ca
concierge@one-wellness.ca 

