 Where is the Achilles tendon, and what does it do?
Where is the Achilles tendon, and what does it do?
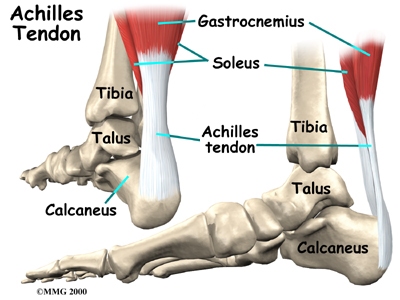
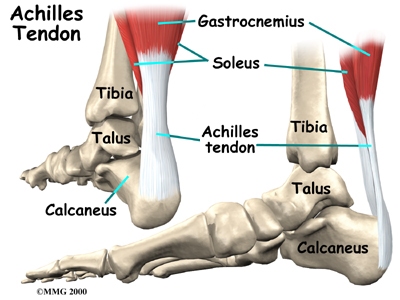
The Achilles tendon is a strong, fibrous band that connects the calf muscle to the heel. The calf is actually formed by two muscles, the underlying soleus and the thick outer gastrocnemius. Together, they form the gastroc-soleus muscle group. The insertion of the gastroc-soleus group into the heel is called the enthesis.
Foot Anatomy Ligaments & Tendons
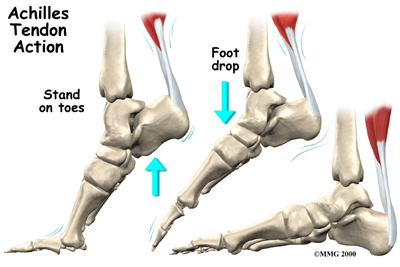
When muscles of the calf contract, they pull on the Achilles tendon, causing your foot to point down and helping you rise up onto your toes. This powerful muscle group is especially active when you sprint, jump, or climb but is also active during every regular step you take. Several different problems can occur that affect the Achilles tendon, some rather minor and some quite severe.
Tendocalcaneal Bursitis
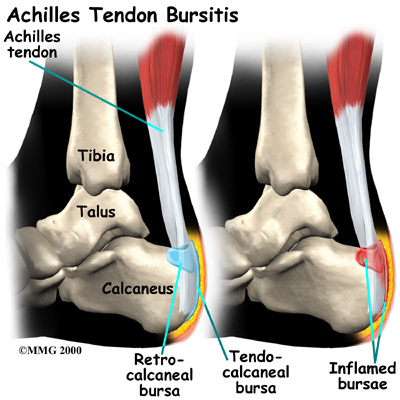
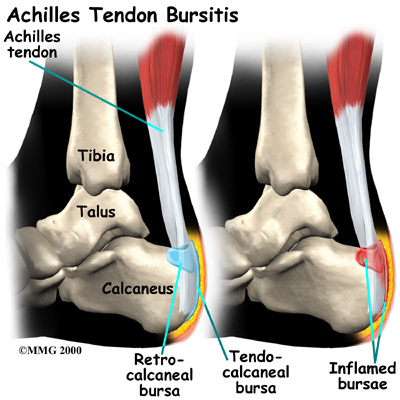
A bursa is a fluid-filled sac designed to limit friction between rubbing body parts. These sacs, or bursae, are found in many places in the body. When a bursa becomes inflamed, the condition is called bursitis. Tendocalcaneal bursitis is an inflammation in the bursa behind the heel bone. This bursa normally limits friction when the thick fibrous Achilles tendon that runs down the back of the calf glides up and down behind the heel. With increased or repetitive activity that causes increased friction, bursitis in this area can develop.
Achilles Tendonitis/Paratendonitis
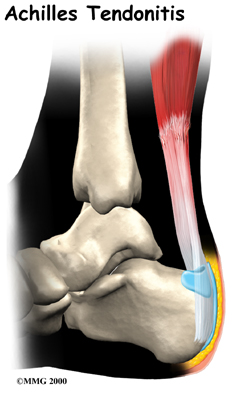
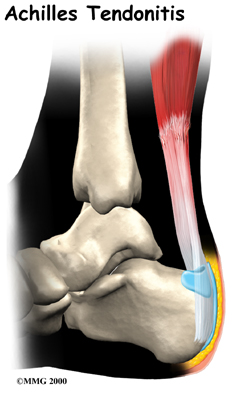 A violent strain can cause trauma to the calf muscles or the Achilles tendon. This injury can happen during a strong contraction of the muscle, as when running or sprinting. Landing on the ground after a jump can force the foot upward, also causing injury. The strain can affect different portions of the calf muscles or Achilles tendon. For instance, the strain may occur in the center of the muscle, or it may happen where the muscles join the Achilles tendon (called the musculotendinous junction). This strain leads to an inflammatory process around the tendon. Initially, it is the irritation of the outer covering of the tendon, called the paratenon, affected by inflammation, which causes paratendonitis. Paratendonitis is simply inflammation in the lining around the tendon. An increase in activity or the commencement of a new activity which the body is not used to can also cause the outer covering to become inflamed. Sometimes even the use of new footwear leads to added strain on the tendon leading to inflammation.
A violent strain can cause trauma to the calf muscles or the Achilles tendon. This injury can happen during a strong contraction of the muscle, as when running or sprinting. Landing on the ground after a jump can force the foot upward, also causing injury. The strain can affect different portions of the calf muscles or Achilles tendon. For instance, the strain may occur in the center of the muscle, or it may happen where the muscles join the Achilles tendon (called the musculotendinous junction). This strain leads to an inflammatory process around the tendon. Initially, it is the irritation of the outer covering of the tendon, called the paratenon, affected by inflammation, which causes paratendonitis. Paratendonitis is simply inflammation in the lining around the tendon. An increase in activity or the commencement of a new activity which the body is not used to can also cause the outer covering to become inflamed. Sometimes even the use of new footwear leads to added strain on the tendon leading to inflammation.
The use of the term tendonitis to describe the common Achilles tendon injury has been disputed in recent years due to the fact that the suffix ‘itis’, in medical terminology, denotes the process of inflammation occurring. Studies have actually shown that in cases of chronic Achilles pain, there are no acute signs of inflammation so it is theoretically incorrect to use the ‘itis’ suffix to describe this injury. The common terminology of tendonitis generally refers to two subsets of separate injuries: paratendonitis, and tendonosis.
Achilles Tendonosis/Tendinopathy
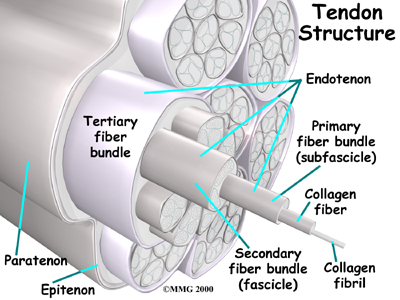
Chronic overuse or long term inflammation may contribute to changes in the Achilles tendon, leading to degeneration and thickening of the tendon. As mentioned above, studies show that although inflammation may have contributed to the initial changes in the tendon, there is no acute sign of inflammation in chronically painful tendons. Most experts now refer to this chronic condition as tendonosis or tendinopathy instead of the acute diagnosis of paratendonitis or tendonitis. Acute inflammation, however, is not a precursor to the development of tendonosis. The degeneration and thickening of the achilles tendon that is the hallmark of a tendonosis diagnosis can also develop over time simply from general wear and tear. Tendons are made up of strands of a material called collagen. (Think of a tendon as similar to a nylon rope and the strands of collagen as the individual nylon strands.) Degeneration in a tendon usually shows up as a loss of the normal arrangement of the fibers of the tendon. Some fibers even break (microtears,) and the tendon loses overall strength.

In these situations the body tries to naturally heal the tendon and this causes the tendon to become thickened as scar tissue and fatty tissue tries to fill in the deficits in the tissue. This process can continue to the extent that a nodule made up of scar tissue forms within the tendon. Tendonosis or tendinopathy is essentially failed healing. It is the accumulation of microscopic injuries over time that do not heal, and then lead to a chronically degenerated tendon. The weakened, degenerative tendon sets the stage for the possibility of actual rupture of the Achilles tendon.
Achilles Tendon Rupture
In severe cases, the force of a violent strain may even rupture the Achilles tendon. The classic example is a middle-aged tennis player or weekend warrior who places too much stress on the tendon and experiences a tearing of the tendon. In some instances, the rupture may be preceded by a period of Achilles paratendonitis, or a tendonosis, which renders the tendon weaker than normal.
Related Document: One Wellness Patient's Guide to Foot Anatomy


 Where is the Achilles tendon, and what does it do?
Where is the Achilles tendon, and what does it do?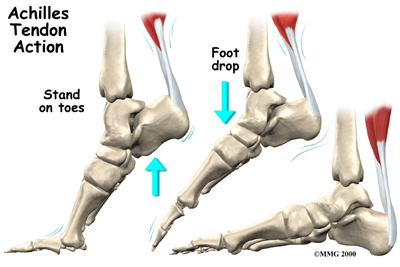
 A violent strain can cause trauma to the calf muscles or the Achilles tendon. This injury can happen during a strong contraction of the muscle, as when running or sprinting. Landing on the ground after a jump can force the foot upward, also causing injury. The strain can affect different portions of the calf muscles or Achilles tendon. For instance, the strain may occur in the center of the muscle, or it may happen where the muscles join the Achilles tendon (called the musculotendinous junction). This strain leads to an inflammatory process around the tendon. Initially, it is the irritation of the outer covering of the tendon, called the paratenon, affected by inflammation, which causes paratendonitis. Paratendonitis is simply inflammation in the lining around the tendon. An increase in activity or the commencement of a new activity which the body is not used to can also cause the outer covering to become inflamed. Sometimes even the use of new footwear leads to added strain on the tendon leading to inflammation.
A violent strain can cause trauma to the calf muscles or the Achilles tendon. This injury can happen during a strong contraction of the muscle, as when running or sprinting. Landing on the ground after a jump can force the foot upward, also causing injury. The strain can affect different portions of the calf muscles or Achilles tendon. For instance, the strain may occur in the center of the muscle, or it may happen where the muscles join the Achilles tendon (called the musculotendinous junction). This strain leads to an inflammatory process around the tendon. Initially, it is the irritation of the outer covering of the tendon, called the paratenon, affected by inflammation, which causes paratendonitis. Paratendonitis is simply inflammation in the lining around the tendon. An increase in activity or the commencement of a new activity which the body is not used to can also cause the outer covering to become inflamed. Sometimes even the use of new footwear leads to added strain on the tendon leading to inflammation.
 It's not entirely clear why these problems develop in some people but not in others. Changes in the normal alignment of the foot and leg are often a large contributing factor. For instance, if your feet are flat or your knees naturally knock together, the alignment of your lower extremities in relation to the pull of gravity downwards will not be anatomically perfect. In these cases the stresses put through your legs and into your foot and heel can lead to excess stress on the Achilles tendon of one or both legs. A similar alignment issue can occur if you have had a previous injury to one leg (i.e.: ankle sprain, bone fracture, hip or back injury.) Previous injuries will often cause you to use your legs differently during everyday activities as the injury heals and you are dealing with pain or decreased range of motion. If the injury is not fully rehabilitated by regaining maximum range of motion, strength, and normal functional movement then muscle imbalances can occur. These muscle imbalances of the hip and leg will then affect your alignment of the forces down your leg and into your foot and heel in everyday activities such as walking, running, jumping, or stair climbing. This can then lead to excessive stress at the Achilles tendon. Tight calf muscles can cause similar problems. Feet that are too rigid can also cause extra stress on the tendon due to poor shock absorption. Anyone with one leg shorter than the other or chronic ligament laxity in the ankle is also at an increased risk of Achilles tendon problems due again to the alignment issue these problems create.
It's not entirely clear why these problems develop in some people but not in others. Changes in the normal alignment of the foot and leg are often a large contributing factor. For instance, if your feet are flat or your knees naturally knock together, the alignment of your lower extremities in relation to the pull of gravity downwards will not be anatomically perfect. In these cases the stresses put through your legs and into your foot and heel can lead to excess stress on the Achilles tendon of one or both legs. A similar alignment issue can occur if you have had a previous injury to one leg (i.e.: ankle sprain, bone fracture, hip or back injury.) Previous injuries will often cause you to use your legs differently during everyday activities as the injury heals and you are dealing with pain or decreased range of motion. If the injury is not fully rehabilitated by regaining maximum range of motion, strength, and normal functional movement then muscle imbalances can occur. These muscle imbalances of the hip and leg will then affect your alignment of the forces down your leg and into your foot and heel in everyday activities such as walking, running, jumping, or stair climbing. This can then lead to excessive stress at the Achilles tendon. Tight calf muscles can cause similar problems. Feet that are too rigid can also cause extra stress on the tendon due to poor shock absorption. Anyone with one leg shorter than the other or chronic ligament laxity in the ankle is also at an increased risk of Achilles tendon problems due again to the alignment issue these problems create.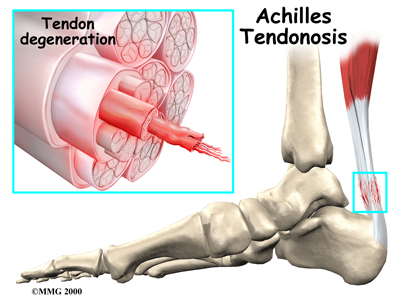 Sudden increases in training intensity can also be a key factor in the development of an overuse Achilles tendon injury. Runners may have recently added on miles or have engaged in excessive hill training. Non-athletes may develop problems if they engage in an unusual amount of walking compared to their normal activity level (i.e.: a day of sightseeing.) Training regularly on cambered surfaces or hard surfaces can also lead to Achilles tendon problems. Other risk factors include obesity or an increase in weight (pregnancy,) diabetes (or other endocrine disorders), exposure to steroids, and taking fluoroquinolones (antibiotics). Shoes that rub on the heel, have inflexible soles, poor support, lack of shock absorption, or that are excessively worn or do not fit well (adding pressure to the heel) can also initiate an Achilles tendon irritation.
Sudden increases in training intensity can also be a key factor in the development of an overuse Achilles tendon injury. Runners may have recently added on miles or have engaged in excessive hill training. Non-athletes may develop problems if they engage in an unusual amount of walking compared to their normal activity level (i.e.: a day of sightseeing.) Training regularly on cambered surfaces or hard surfaces can also lead to Achilles tendon problems. Other risk factors include obesity or an increase in weight (pregnancy,) diabetes (or other endocrine disorders), exposure to steroids, and taking fluoroquinolones (antibiotics). Shoes that rub on the heel, have inflexible soles, poor support, lack of shock absorption, or that are excessively worn or do not fit well (adding pressure to the heel) can also initiate an Achilles tendon irritation.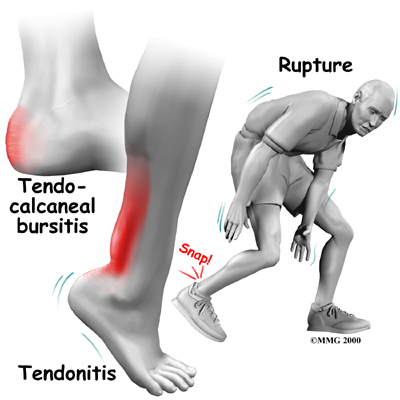
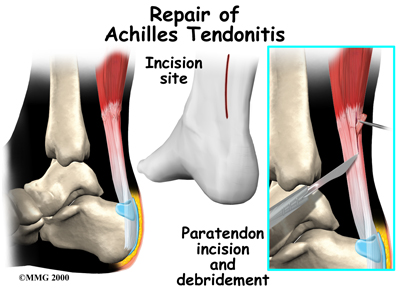 In some cases of persistent tendonitis or tendonosis a procedure called debridement of the Achilles tendon may be suggested to help treat the problem. This procedure is usually done through an incision on the back of the ankle near the Achilles tendon. The tendon is identified, and any inflamed paratenon tissue (the covering of the tendon) is removed. In the case of tendonosis the tendon is then split, and the degenerative portion of the tendon is removed. The split tendon is then repaired and allowed to heal. It is unclear why, but removing the degenerative portion of the tendon seems to stimulate repair of the tendon to a more normal state.
In some cases of persistent tendonitis or tendonosis a procedure called debridement of the Achilles tendon may be suggested to help treat the problem. This procedure is usually done through an incision on the back of the ankle near the Achilles tendon. The tendon is identified, and any inflamed paratenon tissue (the covering of the tendon) is removed. In the case of tendonosis the tendon is then split, and the degenerative portion of the tendon is removed. The split tendon is then repaired and allowed to heal. It is unclear why, but removing the degenerative portion of the tendon seems to stimulate repair of the tendon to a more normal state.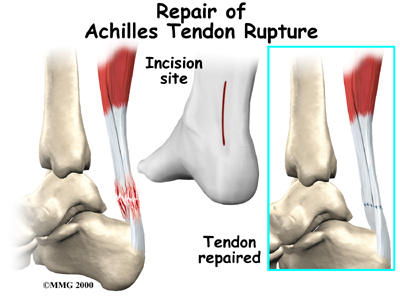
 (403) 679-7179
(403) 679-7179  concierge@one-wellness.ca
concierge@one-wellness.ca 

